Melasma
Melasma is a very common hyperpigmentary disorder that mainly occurs in women, although it can affect men in 10% of cases. This condition is characterized by the appearance of grey-brown patches on sun-exposed areas such as the cheeks,nose bridge, forehead and chin. It can also appear on other parts of the body such as the forearms and neck. Melasma is usually related to a state of hormone excess, such as in pregnancy and with use of birth control pills. In fact, it is so common in pregnancy that it has been dubbed the ‘mask of pregnancy’.
Sun exposure and tanning will make the condition worse. As such, sun protection is crucial in the treatment of melasma. This means using a broad-spectrum sunscreen every day and reapplying it frequently throughout the day. However, sun protection alone is not enough. Patients need to be seen by a dermatologist to assess how deeply the melasma has penetrated the skin. This is done using a special device called a Wood’s lamp. In some cases, a skin biopsy may be required to rule out other similar looking conditions, so that the diagnosis can be confirmed, and appropriate treatment instituted. A skin biopsy is a minor procedure involving removal of a small sample of skin which is then analysed under the microscope.
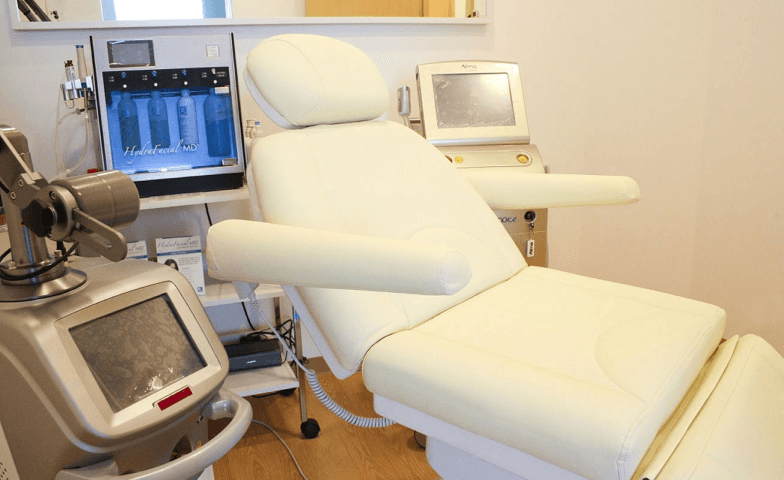
Melasma is challenging to treat as recurrence after initial successful treatment is high. It is best controlled with regular use of broad spectrum suncreens, sun protection and topical creams containing hydroquinone, azelaic acid or kojic acid, which work by lightening the skin. The dermatologist may even prescribe a combination cream containing hydroquinone, retinoid and a steroid in one. In more recalcitrant cases that do not respond to topical treatment, procedures such as intense pulse light (IPL), laser treatment, chemical peels, microdermabrasion and dermabrasion may be offered.
Melasma may fade on its own in some cases e.g. when the trigger is due to conditions such as pregnancy or taking birth control pills. Most cases of melasma can be stubborn. It may take months of treatment to see improvement. However, under the dermatologist care, many patients with melasma have good outcomes. It is important to follow the dermatologist’s advice closely to get the best benefit from treatment.